Glomerulonephritis is inflammation of the tiny filters in your kidneys (glomeruli). Glomeruli remove excess fluid, electrolytes and waste from your bloodstream and pass them into your urine.
If glomerulonephritis occurs on its own, it's known as primary glomerulonephritis. If another disease, such as lupus or diabetes, is the cause, it's called secondary glomerulonephritis.
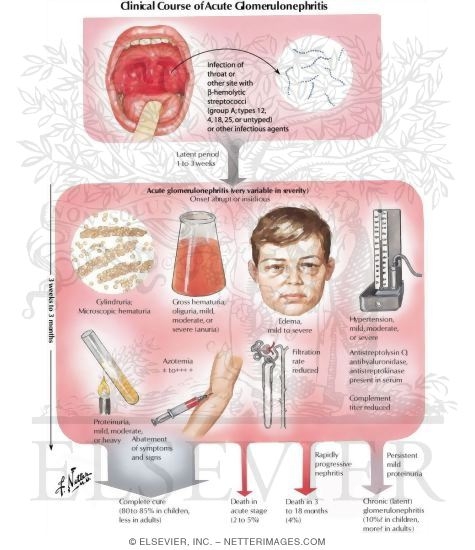
Etiology of AGN
A variety of conditions can cause glomerulonephritis, ranging from infections that affect your kidneys to diseases that affect your whole body, including your kidneys. Sometimes the cause is unknown. Here are some examples of conditions that can lead to inflammation of the kidneys' glomeruli:
· Post-streptococcal glomerulonephritis. Glomerulonephritis may develop a week or two after recovery from a strep throat infection or, rarely, a skin infection (impetigo). An overproduction of antibodies stimulated by the infection may eventually settle in the glomeruli, causing inflammation.
· Viral infections. Among the viral infections that may trigger glomerulonephritis are the human immunodeficiency virus (HIV), which causes AIDS, and the hepatitis B and hepatitis C viruses.
· Lupus. A chronic inflammatory disease, lupus can affect many parts of your body, including your skin, joints, kidneys, blood cells, heart and lungs.
· Goodpasture's syndrome. A rare immunological lung disorder that may mimic pneumonia, Goodpasture's syndrome causes bleeding (hemorrhage) into your lungs as well as glomerulonephritis.
· IgA nephropathy. Characterized by recurrent episodes of blood in the urine, this primary glomerular disease results from deposits of immunoglobulin A (IgA) in the glomeruli. IgA nephropathy can progress for years with no noticeable symptoms. The disorder seems to be more common in men than in women.
Pathophysiology og AGN
In nearly all types of AGN, the epithelial or podocyte layer of the glomerular membrane is disturbed.
Antibody - antigen complexes in the glomerular capillary wall activate biochemical mediators of inflammation- complement leukocyte and fibrin which will attract neutrophils and monocyte, which will release lysosomal enzyme that will damage the glomerular cell walls and cause proliferation.
Symptoms
Protenuria- since the glomerular filtering membrane is damaged big macro-molecules such as protein could pass through and excreted through the urine.
Hypertension- When their is a decrease NaCl filtration (NaCl retention) will stimulate the macula densa to signal the JG cell to release renin hence increasing the blood pressure.
Hematuria- - since the glomerular filtering membrane is damaged blood passes and excreted through the urine.
Edema- Since in glomerulonephritis their is protenuria, albumin is being excreted. Their will be a decreased in oncotic pressure and an increase filtration across the capillary resulting in edema.
Laboratory Test
Specific signs and symptoms may suggest glomerulonephritis, but the condition often comes to light when a routine urinalysis is abnormal. Tests to assess your kidney function and make a diagnosis of glomerulonephritis include:
· Urine test. A urinalysis may show red blood cells and red cell casts in your urine, an indicator of possible damage to the glomeruli. Urinalysis results may also show white blood cells, a common indicator of infection or inflammation, and increased protein, which may indicate nephron damage. Other indicators, such as increased blood levels of creatinine or urea, are red flags.
· Blood tests. These can provide information about kidney damage and impairment of the glomeruli by measuring levels of waste products, such as creatinine and blood urea nitrogen.
· Imaging tests. If your doctor detects evidence of damage, he or she may recommend diagnostic studies that allow visualization of your kidneys, such as a kidney X-ray, an ultrasound examination or a computerized tomography (CT) scan.
· Kidney biopsy. This procedure involves using a special needle to extract small pieces of kidney tissue for microscopic examination to help determine the cause of the inflammation. A kidney biopsy is almost always necessary to confirm a diagnosis of glomerulonephritis.
Management
Antibiotics
Antibiotics (eg, penicillin) are used to control local symptoms and to prevent spread of infection to close contacts. Antimicrobial therapy does not appear to prevent the development of GN, except if given within the first 36 hours. Antibiotic treatment of close contacts of the index case may help prevent development of PSGN.
Other agents
Loop diuretics may be required in patients who are edematous and hypertensive in order to remove excess fluid and to correct hypertension.
Vasodilator drugs (eg, nitroprusside, nifedipine, hydralazine, diazoxide) may be used if severe hypertension or encephalopathy is present.
No comments:
Post a Comment